Some wounds won't heal by themselves. These lesions, which include certain diabetic ulcers, burns and surgical injuries, cause long-term suffering and can linger indefinitely if not successfully treated. They sometimes become infected and in extreme cases turn fatal.
Current chronic wound therapies often require surgery or lead to overuse of antibiotics, which can worsen the problem of antibiotic-resistant bacteria. “Chronic wounds affect tens of millions of people,” says California Institute of Technology biomedical engineer Wei Gao. “There's an urgent need for personalized wound treatment.”
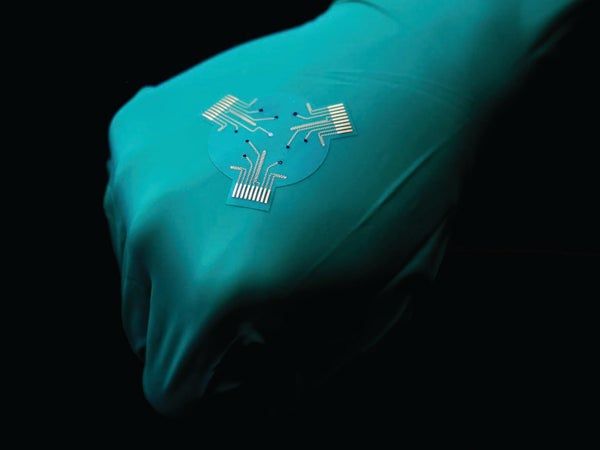
For a study published in Science Advances, Gao and his colleagues used rodents to test a “smart bandage” that could make chronic wound healing easier and faster. It consists of a stretchable polymer patch that adheres to the skin, containing medication and a thin layer of electronics that monitors and wirelessly transmits data about the wound's condition. The patch can carry out controlled delivery of two treatments: a drug and an electric current.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The bandage builds on previous efforts to promote healing with electricity. This process, called electrotherapy, works both by attracting immune cells and skin cells to the wound and by boosting cell growth and division. A study published last year led by engineer Yuanwen Jiang, now at the University of Pennsylvania, described a bandage that monitored temperature and conductivity, using the collected data to control delivery of electrotherapy.
The new research adds biochemical sensing capabilities. In addition to temperature and pH, the bandage's biosensor monitors levels of ammonium, glucose, lactate and uric acid; together these measurements provide information about inflammation, infection and stage of healing. “Biochemical signals open up new opportunities because you're able to really probe what's happening on a molecular level,” Jiang says. “That's the key novelty here.” Gao and his colleagues also added an electroactive gel that releases an anti-inflammatory, antimicrobial drug when stimulated by an electrode. Another electrode stimulates the wound directly.
The team tested the bandage on rodents with diabetic wounds and found that it accurately detected changes in inflammatory and metabolic states at different stages of wound healing. The bandage's combined treatments fully healed rodent wounds in two weeks. Each individual treatment achieved at least partial healing within that time, and untreated animals did not heal.
Researchers still need to investigate the bandage's biosensor durability in human patients' chronic wounds. “Requirements for the lifetime of the device are very different between rodents and human subjects,” Jiang says. “Stability over that extended period has not been tested yet.”
As they head toward human testing, the team is working to improve accuracy and stability. “We hope to apply this smart bandage technology in humans in the next year,” Gao says. “Hopefully the information we get can really benefit people with chronic wounds.”